What is Progressive Supranuclear Palsy (PSP)?
Progressive Supranuclear Palsy (PSP) is a complex neurological condition that progressively affects movement, balance, vision, speech, and swallowing.
PSP disease gets its full name because it progresses and gets worse over time (progressive); it damages the parts of the brain that control eye movements (supranuclear) and causes muscle weakness (palsy).
PSP belongs to a category of disorders called Atypical Parkinsonian Disorders. It often gets misdiagnosed as Parkinson’s disease early on due to some overlapping symptoms like problems with balance, walking, coordination, and eye movements. However, there are distinguishing features and symptoms of PSP, such as prominent early backwards falls, fixed gaze, and more stiffness and slowness. Receiving an early diagnosis provides people with the opportunity to receive more tailored support and symptom management.
READ PAM’S EXPERIENCE
Pam shares details of her husband’s PSP diagnosis and how local support helped him stay independent for as long as possible.
Prevalence and Causes of PSP in the UK
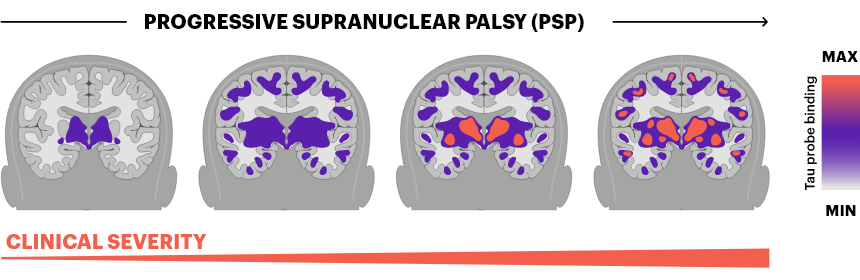
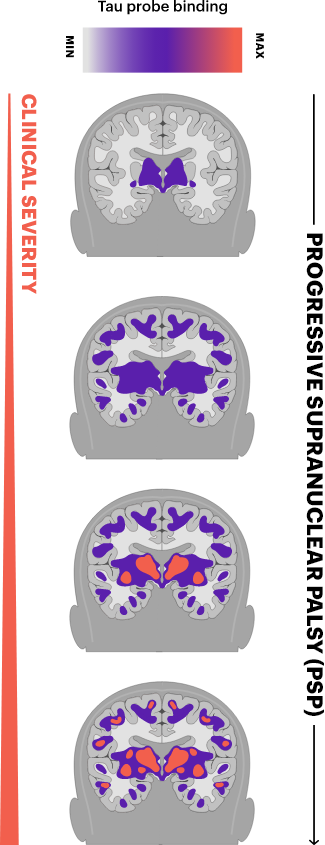
Progressive Supranuclear Palsy (PSP) is a rare neurodegenerative disease caused by the progressive death of nerve cells in certain parts of the brain. Specifically, PSP is associated with the overproduction of a protein called “tau,” which accumulates in and damages brain cells. Researchers are still working to understand the causes of PSP and what exactly triggers this overproduction of tau, but it likely involves a combination of genetic susceptibility factors and unknown environmental exposures or triggers.
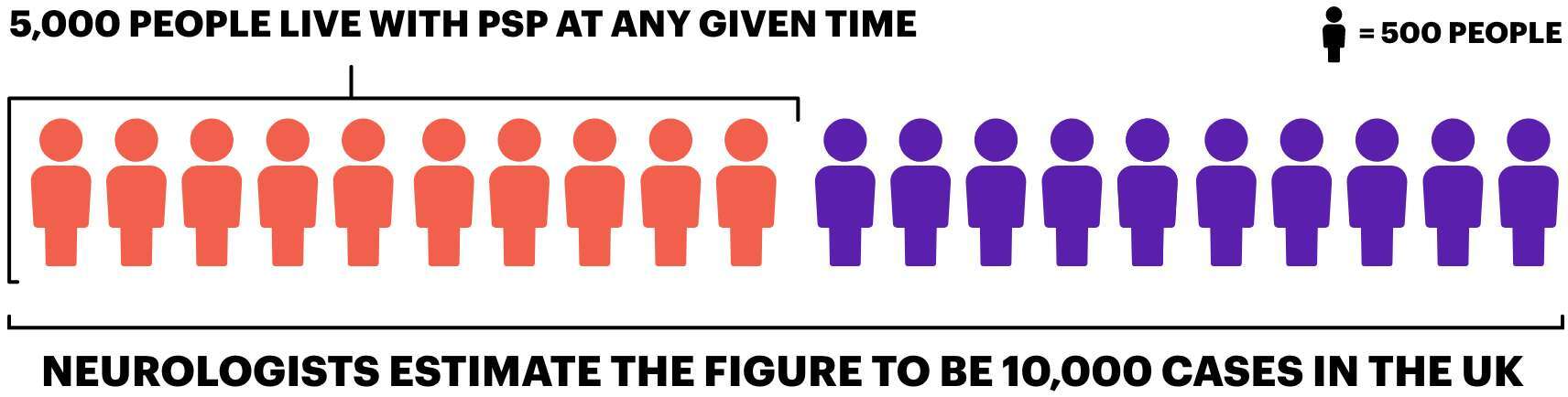
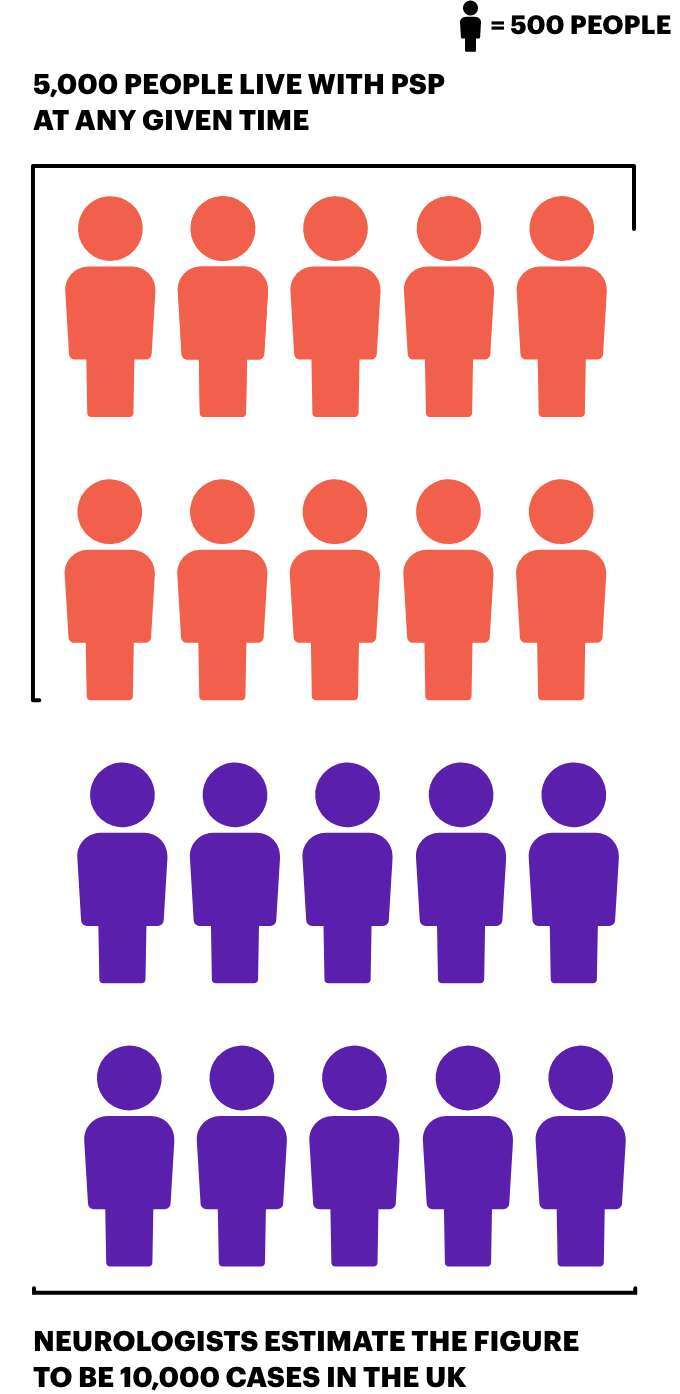
Research into the prevalence of Progressive Supranuclear Palsy (PSP) in the UK estimates around 5,000 people are living with the condition at any given time. However, neurologists believe the actual figure may be as high as 10,000 cases in the UK.
A key reason why estimating prevalence is problematic is that Progressive Supranuclear Palsy (PSP) is extremely hard to diagnose correctly. Around 60% of people are initially misdiagnosed with other conditions, including Parkinson’s disease, a stroke or depression. It can take up to three years from the onset of the first symptoms for someone to receive the correct PSP diagnosis. Currently, there is no definitive test that can be offered to diagnose PSP. A neurologist will gather a person’s medical history and perform a physical examination, looking at the following main symptoms:
The main symptoms used to diagnose PSP include:
- progressive loss of balance
- falls (especially backwards)
- vision issues
- speech changes
- difficulty swallowing
- cognitive changes
- decreased facial expressions
However, PSP affects each person differently. Not everyone experiences all stages and symptoms of Progressive Supranuclear Palsy. This makes recognising and tracking the disease complex. Still, a diagnosis of probable or definite PSP requires gradually emerging symptoms, examination findings confirming brain cell damage consistent with PSP, and ruling out other possible causes.
The difficulties of PSP Diagnosis
Dr Boyd Ghosh speaks on our podcast about the challenges of diagnosing PSP
LISTEN TO THE EPISODE:
Series 2 Episode 2 – Dr Boyd Ghosh talks about diagnosing PSP & CBD
Living with PSP
It can be overwhelming to think about the various ways in which PSP may affect you in the future. Please bear in mind that although there are many PSP symptoms, you may not be affected by everything listed in this section.
Remember that if you need advice on managing a particular symptom, your GP, neurologist, and other members of your healthcare team are there to help.
Symptoms and Effects
Cognition and Mood
Apathy
Lack of enthusiasm for previous interests/hobbies, withdrawal from social activities
Impulsive behaviour
Taking actions without thinking them through, frustration with disability
Mood swings
Inappropriate laughter/crying, exaggerated emotional reactions
Memory problems
Difficulty learning new information and storing new memories
Language problems
Difficulty finding words and expressing complex ideas
Difficulty sequencing thoughts and actions
It is harder to explain events in order and follow multiple-step instructions
Mobility and Falls
Slowed movements
Walking and other motions become slower
Muscle stiffness
Rigidity affecting posture, gait, and range of motion
Poor balance
Unsteadiness when standing or walking
Falls
Sudden loss of balance, often falling backwards and risking injury
Fatigue and Sleep
Overwhelming exhaustion
Lack of energy for basic tasks
Sleep difficulties
Trouble falling or staying asleep, disrupted sleep cycles
Pain
Muscle cramps and spasms
Due to stiffness and rigidity
Headaches or “muzzy” sensations
From neck and back stiffness
Discomfort from posture
Muscle tightness causes discomfort
Secondary pain
From falls, pressure sores, etc.
Speech and Communication
Harsh, strained vocal quality
Reduced speech volume
Difficulty in finding the correct word or words
Slurring of words
Rapid rate of speech
Swallowing, Eating and Drinking
Coughing when eating and drinking
Coughing when eating and drinking
Taking much longer to eat meals
Weight loss
Vision
Double vision
Seeing two images
Blurred vision
Lack of visual clarity
Tunnel vision
Greatly restricted field of view
Slow, jerky eye movements
Difficulty tracking smoothly
Difficulty looking up and down
Problems seeing things above or below
Light sensitivity
Bothered by bright lights
Eyelids close involuntarily
It is hard to keep the eyes open
Bladder and Bowel
Slowed movements
Infrequent/difficult bowel movements
Urinary urgency
Sudden need to urinate
Hesitancy
Trouble starting urination
Incontinence
Inability to control urine flow

Want to know more about PSP?
Download our PDF for a more in depth introduction to PSP & CBD
Who can help?
Most people will see a number of healthcare professionals during their illness. PSP is a rare disease, and because of this, most GPs will only come across one or two people with the condition during their working life. To help you, here is a list of the health and social care professionals who may be involved in your care. As PSP disease varies significantly from person to person, you won’t necessarily meet all of them, and the list isn’t meant to be exhaustive.
Healthcare professionals available to support you may include:
General Practitioner (GP)
The primary carer responsible for looking after the person’s health. Refers them to other services like hospitals or specialists when needed.
Multi-Disciplinary Team (MDT)
A group of various health and social care professionals who work together to coordinate care and treatment tailored to the individual.
Neurologist
Specialises in conditions of the brain and nerves. They help diagnose, manage symptoms and assess care needs
Occupational Therapist (OT)
Helps the person continue daily activities independently. Gives advice on fall prevention, fatigue management, mobility aids, home adaptations.
Dietitian
Works with the speech and language therapist to advise on diet and maintaining weight as well as advice on tube feeding
Orthoptist and Ophthalmologist
Assess and treat vision/eye movement issues. Recommend exercises, and lenses.
Speech and Language Therapist
Assess communication issues and recommend communication aids. Works with a dietitian on swallowing difficulties.
Palliative Care Team
As PSP progresses, palliative care becomes essential for relieving symptoms and improving quality of life. This care includes pain management, nutritional support, and addressing psychological and spiritual needs.
Physiotherapists
Physiotherapists can design specific exercises that help maintain muscle strength and flexibility, which can prolong independence in daily activities and prevent falls
Read Claire’s Experience
Claire talks about the symptoms her mum was experiencing ahead of her PSP diagnosis and how they finally got answers.
General Benefits and Entitlements
There is a range of disability-related financial support, including benefits for specific needs, tax credits, direct financial support and entitlements enabling you to claim other types of financial support.
We have outlined all of these in an information sheet. This will give you an overview of the various benefits and entitlements available and how and where to apply for them.
These benefits are not means-tested and are determined by specific criteria related to the illness/disability. Help with completion of forms can be provided by the Department of Work and Pensions Home Visiting Service.
Caring for someone with PSP
Caring for someone with PSP involves understanding various stages and adapting to changing needs. Initial shock and adjustment to the caregiving role are common, as is the feeling of loss regarding future plans and relationship changes. Acceptance and finding a routine in caregiving are crucial, alongside managing personal health and wellbeing.
It’s important to recognise the need for and seek practical help, like a Carer’s Assessment, and to balance work with caregiving responsibilities. Support from organisations like PSPA, offering emotional support, and connections to others in similar situations, is invaluable.
At PSPA, we have numerous resources to offer support to caregivers. We are committed to ensuring that family and unpaid carers of all ages who support people with PSP have access to a network of support and high-quality, reliable information.
Find local support and advice here.
What can be expected in later life?
Navigating the later stages of life with Progressive Supranuclear Palsy involves addressing several key areas. These include exploring respite care options for short-term relief and extended stays, understanding the intricacies of continuing healthcare, and preparing for end-of-life decisions.
Legal matters such as advance decisions to refuse treatment, power of attorney, and making a will are vital for ensuring personal wishes are honoured.
Additionally, considering brain tissue donation and planning for funerals are significant. PSPA offers support in these areas, providing essential guidance and resources for individuals and their families during this challenging phase of life. Discover more about advanced planning with our podcast interview with Ewan Phillips.
Listen to the episode
Series 1 Episode 8 – Advance Care Planning with Ewan Phillips
Download our PDF for more information on advance decision guidance for people living with PSP & CBD.
Learn more about PSP and how it progresses
Download our PDF for a more information on how to navigate life with PSP as the condition progresses.
How can PSPA help?
Currently, PSPA is the only UK charity dedicated to creating a better future for everyone affected by PSP & CBD. In 2023, we introduced a new charity strategy to help focus any developments of our support services, information, awareness raising or research.
Our goals from the strategy are to:
- Enable people living with PSP & CBD and their families to live their best lives possible with high-quality support and information.
- Improve the quality of life of people living with PSP & CBD through research, education and awareness-raising.
- Put the voice of people living with PSP & CBD at the heart of what we do.
Watch the video below to hear our CEO talk about our strategy.
Overall, we aim to create a better future for everyone affected by PSP & CBD. We strive to improve diagnosis and discover treatment and, ultimately, a cure.
Frequently Asked Questions
What causes Progressive Supranuclear Palsy (PSP)?
The exact cause of PSP is unknown. In people living with PSP, the tau protein in the brain is not broken down properly and forms harmful clumps in brain cells, which stop them from working properly. Once PSP has started, brain cells in certain parts of the brain die because of this build-up of the tau protein.
How is Progressive Supranuclear Palsy (PSP) diagnosed?
A definite diagnosis of PSP can only be established at post-mortem. A suspected or probable PSP diagnosis can be given following a mixture of clinical observations, brain scans, gradually emerging symptoms, and ruling out other possible causes.
Is there a cure or treatment for PSP?
Currently, there is no treatment to help slow the development of Progressive Supranuclear Palsy or cure the disease completely. However, supportive care options are available to help manage symptoms.
What is the difference between PSP disease and Parkinson’s disease?
PSP belongs to a category of disorders called Atypical Parkinsonian Disorders. While it is often misdiagnosed as Parkinson’s, there are some distinguishing PSP symptoms, such as prominent early backwards falls, fixed gaze, and more stiffness and slowness. PSP also progresses faster and does not respond well to Parkinson’s medications.
What is the life expectancy with Progressive Supranuclear Palsy (PSP)?
It is common to read that life expectancy is six to seven years from the onset of PSP, but this figure does not consider how variable the condition is.
Is Progressive Supranuclear Palsy (PSP) genetic?
Less than 1% of people diagnosed with PSP have a family member with the same condition. Unlike some other neurological conditions, there does not seem to be a single genetic cause of PSP. However, the role of genetics in PSP is currently under investigation.
What kind of support is available for people living with PSP, their carers and families?
As the only UK charity for PSP, PSPA offers a range of support services to people living with the condition, their carers and family members. These include a dedicated PSPA Helpline service, regional and online Support Groups, Link Volunteer service, PSPA Support Grants, and various information resources. You may also get support from external resources like Adult Social Care, local carer organisations, and specialist palliative care services, among others.


